Patient-centered care is a transformative approach in the healthcare landscape that prioritizes the individual needs, preferences, and values of patients. This model shifts the focus from a purely clinical perspective to one that encompasses the holistic experience of the patient. It emphasizes the importance of understanding the patient’s unique circumstances, including their emotional, social, and psychological needs.
By fostering a collaborative relationship between healthcare providers and patients, this approach aims to enhance the quality of care and improve health outcomes. The evolution of patient-centered care has been driven by a growing recognition that effective healthcare extends beyond mere diagnosis and treatment. It involves engaging patients as active participants in their own care journey.
This paradigm shift has been supported by various frameworks and guidelines, such as the Institute of Medicine’s six aims for healthcare improvement: safety, effectiveness, patient-centeredness, timeliness, efficiency, and equity. As healthcare systems increasingly adopt this model, the integration of technology, particularly artificial intelligence (AI), is poised to play a pivotal role in enhancing patient-centered care.
Key Takeaways
- Patient-centered care puts the patient at the center of healthcare decision-making, focusing on their individual needs and preferences.
- AI plays a crucial role in healthcare by analyzing large amounts of data to improve diagnosis, treatment, and patient outcomes.
- Generative models are AI systems that can create new data, such as images, text, or audio, based on patterns learned from existing data.
- AI-powered generative models are transforming patient-centered care by personalizing treatment plans and improving communication between patients and healthcare providers.
- AI enhances diagnosis and treatment by analyzing patient data to identify patterns and provide more accurate and timely interventions.
The Role of AI in Healthcare
Artificial intelligence has emerged as a powerful tool in healthcare, offering innovative solutions that can streamline processes, enhance decision-making, and improve patient outcomes. AI encompasses a range of technologies, including machine learning, natural language processing, and computer vision, which can analyze vast amounts of data to identify patterns and generate insights. In the context of healthcare, AI can assist in various domains such as diagnostics, treatment planning, and operational efficiency.
One of the most significant contributions of AI in healthcare is its ability to process and analyze large datasets quickly and accurately. For instance, AI algorithms can sift through electronic health records (EHRs), clinical notes, and imaging data to identify trends that may not be immediately apparent to human clinicians. This capability not only aids in diagnosing conditions but also helps in predicting patient outcomes and personalizing treatment plans.
Moreover, AI can facilitate administrative tasks, such as scheduling appointments and managing billing processes, allowing healthcare professionals to focus more on direct patient care.
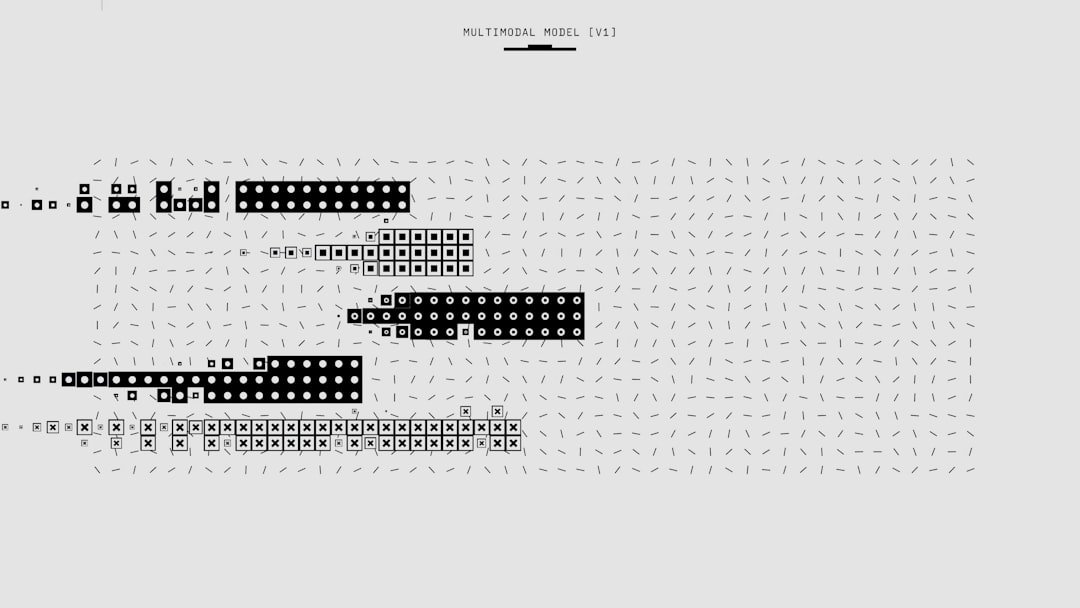
Understanding Generative Models
Generative models represent a class of machine learning algorithms that are designed to generate new data instances that resemble a given dataset. Unlike discriminative models, which focus on classifying existing data points, generative models learn the underlying distribution of the data and can create new samples from that distribution. This capability has profound implications for various applications in healthcare, particularly in enhancing patient-centered care.
One prominent example of generative models is Generative Adversarial Networks (GANs), which consist of two neural networks—the generator and the discriminator—that work against each other to improve their performance. The generator creates new data samples while the discriminator evaluates them against real data. Through this adversarial process, both networks improve over time, leading to high-quality synthetic data generation.
In healthcare, generative models can be used to create realistic patient simulations for training purposes or to augment datasets for rare diseases where data scarcity is a challenge.
How AI-Powered Generative Models are Revolutionizing Patient-Centered Care
AI-powered generative models are revolutionizing patient-centered care by enabling more personalized and effective treatment strategies. These models can analyze vast amounts of patient data to identify patterns that inform tailored interventions. For instance, by generating synthetic patient profiles based on real-world data, healthcare providers can better understand how different demographics respond to various treatments.
This understanding allows for more precise recommendations that align with individual patient needs. Moreover, generative models can enhance clinical decision-making by providing predictive analytics that inform treatment pathways. For example, an AI system could analyze historical treatment outcomes for similar patients and generate recommendations for optimal therapies based on predicted responses.
This not only improves the likelihood of successful outcomes but also empowers patients by involving them in discussions about their care options based on data-driven insights.
Enhancing Diagnosis and Treatment with AI
The integration of AI into diagnostic processes has significantly improved accuracy and efficiency in identifying medical conditions. Traditional diagnostic methods often rely on subjective interpretations of symptoms and test results; however, AI algorithms can analyze complex datasets with greater precision. For instance, AI systems trained on imaging data can detect anomalies in X-rays or MRIs that may be overlooked by human radiologists.
This capability not only enhances diagnostic accuracy but also reduces the time required for interpretation. In treatment planning, AI can assist clinicians by providing evidence-based recommendations tailored to individual patient profiles. By analyzing a patient’s genetic information alongside clinical history and treatment responses from similar cases, AI can suggest personalized treatment regimens that maximize efficacy while minimizing adverse effects.
This level of customization is particularly beneficial in fields such as oncology, where treatment responses can vary significantly among patients with similar diagnoses.
Improving Patient Engagement and Communication
Effective communication is a cornerstone of patient-centered care, and AI technologies are enhancing this aspect by facilitating better interactions between patients and healthcare providers. Chatbots and virtual health assistants powered by natural language processing can provide patients with immediate responses to their inquiries, schedule appointments, and offer medication reminders. These tools not only improve accessibility but also empower patients to take an active role in managing their health.
Furthermore, AI-driven platforms can analyze patient feedback and sentiment from various sources—such as surveys, social media interactions, and online reviews—to gauge overall satisfaction with care experiences. By understanding patient perspectives more comprehensively, healthcare organizations can make informed adjustments to their services and communication strategies. This responsiveness fosters a culture of engagement where patients feel valued and heard.
Personalizing Care Plans with AI
Personalization in healthcare is increasingly becoming a reality thanks to AI technologies that analyze diverse datasets to create individualized care plans. By integrating information from EHRs, genetic testing results, lifestyle factors, and social determinants of health, AI systems can generate comprehensive profiles that inform tailored interventions. For example, a patient with diabetes may receive a personalized care plan that includes specific dietary recommendations based on their unique metabolic profile and lifestyle preferences.
Moreover, AI can continuously learn from ongoing patient interactions and outcomes to refine these care plans over time. As new data becomes available—such as changes in a patient’s condition or response to treatment—the AI system can adjust recommendations accordingly. This dynamic approach ensures that care remains relevant and effective throughout the patient’s journey.
Addressing Healthcare Disparities with AI-Powered Generative Models
Healthcare disparities remain a significant challenge globally, often resulting from socioeconomic factors, geographic location, and systemic biases within healthcare systems. AI-powered generative models have the potential to address these disparities by providing insights into underserved populations and identifying barriers to access. By analyzing demographic data alongside health outcomes, these models can highlight areas where interventions are needed most.
For instance, generative models can simulate potential outcomes for different intervention strategies within specific communities, allowing policymakers to allocate resources more effectively. Additionally, these models can help design targeted outreach programs that address the unique needs of diverse populations. By leveraging AI in this manner, healthcare systems can work towards achieving equity in health outcomes across different demographic groups.
Ethical Considerations in AI-Powered Patient-Centered Care
The integration of AI into patient-centered care raises important ethical considerations that must be addressed to ensure responsible implementation. One primary concern is the potential for bias in AI algorithms, which can arise from training data that does not adequately represent diverse populations. If left unaddressed, such biases could exacerbate existing disparities in healthcare access and outcomes.
Another ethical consideration involves patient privacy and data security. The use of AI necessitates access to sensitive health information; therefore, robust measures must be implemented to protect patient confidentiality while still enabling meaningful analysis. Transparency in how AI systems make decisions is also crucial; patients should be informed about how their data is used and how it influences their care plans.
Overcoming Challenges and Barriers in Implementing AI in Healthcare
Despite the promising potential of AI in enhancing patient-centered care, several challenges hinder its widespread adoption within healthcare systems. One significant barrier is the lack of interoperability among different health information systems. Many organizations use disparate EHR platforms that do not communicate effectively with one another, making it difficult for AI algorithms to access comprehensive datasets necessary for accurate analysis.
Additionally, there is often resistance from healthcare professionals who may be skeptical about relying on technology for clinical decision-making. Education and training are essential to alleviate these concerns; clinicians must understand how AI tools complement their expertise rather than replace it. Furthermore, regulatory frameworks need to evolve alongside technological advancements to ensure safe and effective use of AI in clinical settings.
The Future of Patient-Centered Care with AI-Powered Generative Models
Looking ahead, the future of patient-centered care is poised for significant transformation through the continued integration of AI-powered generative models. As these technologies advance, they will enable even greater personalization of care plans and enhance clinical decision-making processes. The ability to generate synthetic data will also facilitate research into rare diseases and complex conditions where traditional data collection methods fall short.
Moreover, as healthcare systems increasingly embrace telemedicine and remote monitoring solutions, AI will play a crucial role in maintaining continuity of care for patients outside traditional clinical settings. By harnessing real-time data from wearable devices and mobile applications, AI can provide timely insights that inform proactive interventions. In conclusion, the intersection of artificial intelligence and patient-centered care represents a frontier filled with potential for improving health outcomes while addressing systemic challenges within healthcare systems.
As stakeholders navigate this evolving landscape, collaboration among technologists, clinicians, policymakers, and patients will be essential to realize the full benefits of these innovations while ensuring ethical considerations remain at the forefront of implementation efforts.